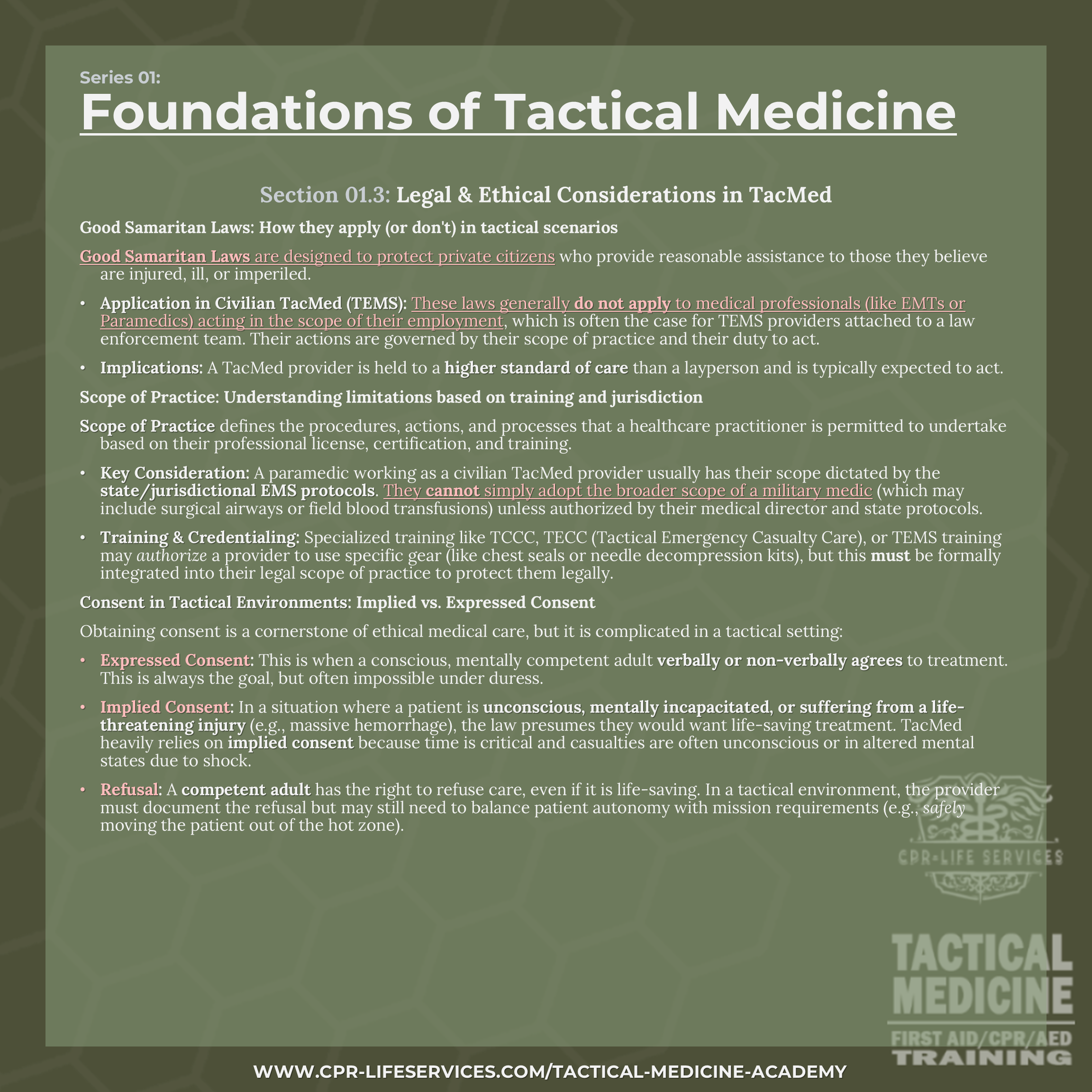
Legal & Ethical Considerations in TacMed
Good Samaritan Laws: How they apply (or don't) in tactical scenarios
Good Samaritan Laws are designed to protect private citizens who provide reasonable assistance to those they believe are injured, ill, or imperiled.
Application in Civilian TacMed (TEMS): These laws generally do not apply to medical professionals (like EMTs or Paramedics) acting in the scope of their employment, which is often the case for TEMS providers attached to a law enforcement team. Their actions are governed by their scope of practice and their duty to act.
Implications: A TacMed provider is held to a higher standard of care than a layperson and is typically expected to act.
Scope of Practice: Understanding limitations based on training and jurisdiction
Scope of Practice defines the procedures, actions, and processes that a healthcare practitioner is permitted to undertake based on their professional license, certification, and training.
Key Consideration: A paramedic working as a civilian TacMed provider usually has their scope dictated by the state/jurisdictional EMS protocols. They cannot simply adopt the broader scope of a military medic (which may include surgical airways or field blood transfusions) unless authorized by their medical director and state protocols.
Training & Credentialing: Specialized training like TCCC, TECC (Tactical Emergency Casualty Care), or TEMS training may authorize a provider to use specific gear (like chest seals or needle decompression kits), but this must be formally integrated into their legal scope of practice to protect them legally.
Consent in Tactical Environments: Implied vs. Expressed Consent
Obtaining consent is a cornerstone of ethical medical care, but it is complicated in a tactical setting:
Expressed Consent: This is when a conscious, mentally competent adult verbally or non-verbally agrees to treatment. This is always the goal, but often impossible under duress.
Implied Consent: In a situation where a patient is unconscious, mentally incapacitated, or suffering from a life-threatening injury (e.g., massive hemorrhage), the law presumes they would want life-saving treatment. TacMed heavily relies on implied consent because time is critical and casualties are often unconscious or in altered mental states due to shock.
Refusal: A competent adult has the right to refuse care, even if it is life-saving. In a tactical environment, the provider must document the refusal but may still need to balance patient autonomy with mission requirements (e.g., safely moving the patient out of the hot zone).
Section 01.3 (Graphic)